Key Points
-
Details the importance of appropriate management of patients attending emergency out of hours clinics.
-
Highlights the continued inappropriate use of antibiotics for treating certain conditions.
-
Demonstrates that there exists a poor understanding of clinical and best practice guidelines among some clinicians with respect to the examination and management of emergency patients.
Abstract
Aim To investigate the clinical management of patients attending for emergency dental treatment.
Design A retrospective analysis of clinical record cards.
Method Information was collected from patient record cards concerning the patient's reason for attendance and their management at an emergency dental clinic in South Sefton, Liverpool.
Results Over a nine month period, 1,718 patients attended the clinic; 1,472 record cards were analysed. Over 80% of the patients attending the out of hours (OOH) clinic had pain associated with a localised dental infection or dental abscess. Where a diagnosis was recorded, only 67% of patients received appropriate treatment. Over 50% of patients received antibiotics alone with no other definitive treatment provided. The principal antibiotic prescribed for both adult and child patients was amoxicillin.
Conclusion The current study has highlighted that GDPs working within the OOH services are not adhering to current clinical and best practice guidelines with respect to patient examination, diagnosis, management, in particular the correct prescribing of antibiotics for dental infections, and clinical record keeping.
Similar content being viewed by others
Introduction
Prior to the inception of the new National Health Service (NHS) dental contact in April 2006, patients were registered with a general dental practitioner who was responsible for their continuing care, including out of surgery hours emergency care. Since April 2006, patients are no longer registered with a dentist and the responsibility for the management of patients not undergoing a course of treatment but requiring urgent treatment rests with the primary care trusts (PCTs). The provision of urgent treatment for all patients outside normal working hours also rests with the PCTs. PCTs have an obligation to provide out of hours emergency dental services for all patients within their area.1
Patients who require urgent care have been clearly defined by the Department of Health1 as those patients who present with:
-
Severe dental and facial pain not controlled by over-the-counter preparations
-
Dental and soft tissue acute infections
-
Uncontrollable dental haemorrhage following extractions
-
Dental trauma
-
Rapidly increasing facial swelling.
The latter three categories require emergency treatment in order to minimise the risk of serious medical complications or prevent long-term dental complications to the patient.
Previous research into out of hours (OOH) emergency services has shown a high level of antibiotic prescribing with little evidence of definitive treatment; approximately 50% of patients attending emergency dental services (EDS) clinics received antibiotics.3,4,5 Antibiotics are prescribed in dental practice therapeutically as an adjunct to the management of dental infections, and until recently prophylactically to prevent metastatic infections such as infective endocarditis.
Prescriptions issued by general dental practitioners (GDPs) account for approximately 7.5% of all antibiotics prescribed in the community.6 Department of Health statistics for the period 1993-2005 show an increasing trend in the number of prescriptions issued by GDPs over this period.7
Previous studies looking at the provision of urgent dental care have failed to investigate the clinically presenting conditions of patients attending such clinics, the recorded diagnosis and the appropriateness of the treatment provided, particularly in relation to the prescribing of antibiotics.4,8,9,10,11,12,13 From these previous studies it was impossible to ascertain whether the antibiotics prescribed to patients attending the OOH clinics was appropriate or not. Casual communications from dentists and patients who have accessed the OOH service suggest that there is an increasing reliance on prescribing antibiotics to manage urgent treatment, rather than provide definitive best practice clinical treatment.
With the drive towards high quality, patient safety and value for money by the Department of Health, along with the recognition of the increasing problem of antimicrobial resistance,14,15,16 there is a need for PCTs to ensure that they are delivering quality care to patients utilising their OOH services and also value for money.
The aims of this current study were to investigate the clinical management of patients attending an out of hours dental clinic under the new NHS dental contract by evaluating their clinical presentation and management and the appropriateness of treatment delivered against established guidelines, particularly with reference to the prescribing of antibiotics.
Materials and methods
The study was designed as a retrospective examination of record cards of patients who accessed and received treatment at the OOH dental clinic in South Sefton between April 2006 and December 2006. This period incorporates the interception of the new dental contract and we aimed to analyse the records of approximately 1,000 consecutive patients attending for dental assessment.
Data collection
Information regarding patient attendance at the OOH dental clinic is recorded on daily triage sheets. Triage sheets for each day of the study period were obtained from the Liverpool Dental Directorate and coded to maintain anonymity. Clinical record cards were identified, retrieved from storage and analysed. Data from each record card was collected and collated on a pro forma specifically designed for the study.
The information collected included:
-
Age and gender of the patient
-
The number of times the patient had utilised the OOH service during the past three years
-
The reason for the patient's attendance
-
The medical history (if relevant)
-
The diagnosis made by the clinician
-
Whether of not treatment options were discussed
-
The treatment provided
-
Any medicines prescribed.
The reasons for patient attendance were classified as pain, swelling, pain together with swelling, a cavity or broken tooth, lost restoration (including crowns and bridges), gingival bleeding, trauma, persistent haemorrhage and 'other' reasons. Each complaint was coded and recorded.
Each patient's medical history was analysed for any potential problems that may have affected their management at the clinic. Medical conditions were coded and recorded.
Simple 'yes' or 'no' answers were recorded on the data sheet to denote whether a diagnosis had been made and recorded, if treatment options had been discussed, and if a prescription was issued. A space was left to record, in their own words, the dentists' diagnosis, treatment provided and details of any prescriptions issued including the generic name of each medicine prescribed, its dosage and duration. These were grouped and coded for analysis.
Statistical analysis
Data was numerically coded and entered into the Statistical Package for Social Sciences (SPSS) Version 15.0 for Windows™. Summary statistics were calculated to include frequencies, percentages and means where indicated.
Ethical approval
Following submission of the protocol to the Sefton Research Committee it was advised that ethical approval was not required for this study.
Results
During the study period 238 clinical sessions were held, with clinical sessions from 18:00 to 22:00 Monday to Sunday with an additional session from 09.00 until 13.00 on both Saturdays and Sundays. Eleven different dentists worked in the emergency dental clinic on a weekly rota system, with most dentists working more than one weekly session during the study period. There were seven male and four female dentists.
For the allocated study period, 1,718 patients were offered appointments to see the on call dentist at the OOH clinic. 1,472 (85.7%) of these patients' record cards were analysed in-depth. The remaining 246 (14.3%) were discarded; 156 record cards were missing, 57 patients failed to attended or were unable to attend their appointment, 18 record cards were incomplete, 14 were illegible and one patient declined treatment on arrival.
The mean number of patients attending the clinics per session was 7.1 (range 0-15). Where data were available there were 801 male (52.4%) and 728 female (47.6%) patients, of whom 1,251 (79%) were adults and 332 (21%) children (ie below the age of 19 years).
1,227 (84%, n = 1,472) patients had only utilised the OOH service once during the three year period. The remaining patients (16.7%) had used the service more than once and in one instance the service had been used six times by the same person.
Relevant medical history
Analysis of the results for patients' medical histories showed 43 patients had medical problems which may have influenced the treatment they received. Seven patients had heart murmurs, four were receiving warfarin therapy, one had a history of rheumatic fever and one a prosthetic heart valve. Twenty-four patients reported an allergy to penicillin, three were pregnant, one was undergoing chemotherapy, and two were taking methotrexate and carbamezipine respectively. Only 19 of these patients received definitive treatment. The rest were treated with antibiotics alone.
Reasons for attendance
Table 1 shows patients' reasons for attendance at the OOH dental clinic. 1,201 patients (adult: 959/1,167, 82.2%; child: 242/305, 79.3%) presenting at the clinic complained of pain, including pain and swelling. One hundred and forty-three patients presented with a swelling alone (adult: 112/1,167, 9.6%; child: 31/305, 10.2%). This included both localised and diffuse facial swellings.
The proportion of patients who were recorded as having a cavity (adult: 75/1,167, 6.2%; child: 8/305, 2.6%) or a lost restoration (including crowns and bridges) was higher in adults than in children. One 93-year-old female patient presented with persistent bleeding following an extraction earlier that day.
More children than adults presented to the clinic with complaints of dental trauma (adult: 10/1,167, 0.9%; child: 19/305, 6.2%). Trauma included both dental and facial trauma. There were nine cases (adult: 5/1,167, 0.4%; child: 4/305, 1.3%) where patients attended for 'other' reasons; these included four cases of broken orthodontic appliances and two cases of black hairy tongue. No clear clinical complaint or diagnosis was recorded for the other three cases.
Clinical diagnosis
Based on clinical findings, a definitive diagnosis was made in 957 (65.0%, n = 1,472) cases.
The most common clinical diagnosis made was caries (23.9%; 254/1,062), followed by cavities caused through decay or lost restorations (17.6%), acute periapical periodontitis (12.1%) and fractured teeth (8.0%). These proportions were higher in children than in adults. A significant proportion of patients also presented with periodontal infections (6.0%), dental abscesses (6.2%), dry sockets (alveolar osteitis) (4.5%), pericoronitis (4.3%) and retained roots (3.7%).
Treatment provided
Treatment options were discussed in 238 (16.2%) cases out of the valid 1,472 record cards.
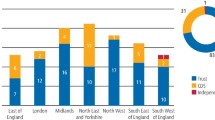
Figures 1 and 2 show how patients attending the OOH clinic were managed and the different treatments provided by the on call dentist. Forty-eight (3.3%) patients who attended the clinic in pain declined any treatment offered. Fifty-two patients were given advice only.
The issuing of an antibiotic prescription alone was the only and most frequent treatment that 438 (37.6%) of adult and 119 (39.0%) of child patients received. Antibiotic therapy together with an active surgical intervention was received by a similar proportion of adult and child patients.
The proportion of patients receiving extractions and surgical drainage of swellings was higher in adults (20.6% and 1.2% respectively) than in children (1.2% and 0.3% respectively). A similar proportion of adults and children underwent endodontic treatment. Approximately 25% of patients received dressings for lost restorations, tooth fractures and dry sockets. One hundred and fifteen patients received a variety of treatments which included curettage around partially erupted 8s or adjustments to appliances/fillings.
Details of prescriptions issued
Analysis of the data showed that 790 (790/1,472, 53.7%) patients received prescriptions. Seven hundred and sixty-five (96.8%) of these were for antibiotics alone or antibiotics in combination with analgesics or mouthwashes. Other prescriptions issued were for analgesics such as dihydrocodeine, ibuprofen and paracetamol; mouthwashes, namely chlorhexidine gluconate (Corsodyl™); and antifungal lozenges and rinses such as Diflam™.
For both adult and child patients, the most frequently prescribed antibiotic was amoxicillin (347/765, 45.6%) followed by metronidazole (247/765, 32.3%). Tetracycline, clindamycin and combinations of antibiotics with clindamycin were only prescribed for adult patients.
Antibiotics prescribed for pain
Table 2 shows the distribution of antibiotics prescribed against the clinical diagnosis made by the clinician for both adults and children. In 57.4% of cases antibiotics were prescribed where no diagnosis was even documented.
Although a definitive diagnosis was not made in many cases it can be speculated that caries, lost fillings and dentoalveolar abscesses were attributable to the cause of dental pain in nearly three quarters of the child patients (143/200, 71.5%). Other significant causes of pain were dry sockets, retained roots, pulpitis and periodontal infections. Antibiotics were prescribed for almost half of these children (49.2%). The same diagnosis was attributed to nearly half of the adult patients with pain (364/757, 48.1%); over a third received an antibiotic prescription (142/364, 39.0%). One hundred and twelve adult patients who complained of pain had an acute apical infection; 77 (68.8%) of these received antibiotic prescriptions alone and only 14 received any adjunctive treatment such as extirpation or extraction of the offending tooth, or the incision of a swelling.
Appropriateness of treatment provided
Analysis of patient management against best practice or evidence-based guidelines showed that 67.7% (n = 957) of patients received treatment that was considered appropriate. Cases that were excluded from this analysis were those where no diagnosis had been made and where patients refused definitive treatment.
Discussion
The study was designed to investigate the management of patients attending the OOH emergency dental clinic in South Sefton, Liverpool, following the inception of the new dental contract in April 2006.
It is well recognised that PCTs are formally responsible for ensuring that appropriate out of hours, emergency and urgent dental service arrangements are in place for their residents and visitors. A PCT also has a duty to ensure value for money and that patients accessing the service receive quality care.1
Dental triage systems exist to prioritise patients who need immediate attention where a delay could compromise their treatment or their health. The OOH clinic in this study employs a second level triage system.1 Managing patients in this way means that effective dental advice can be provided for a large area with limited resources. Likewise, individuals with a clinical need for treatment will be seen promptly and the time of the dental clinician will be used to the greatest effect.
Eighty-five percent of the patient record cards collected during the nine month study period were analysed in-depth for the purpose of the study. Those discarded on the grounds of being missing, incomplete or illegible clearly highlight the ongoing medico-legal issues which continue to surround clinical record keeping and storage.17
Of some concern were the numbers of cases where no clinical diagnosis was made (35.0%) or where treatment options were not documented in the record cards (83.8%). This is not to say that treatment options were not discussed with the patients and simply not documented, but the findings clearly highlight poor compliance with current clinical guidelines and medical record keeping.17
As shown in previous research, the majority of patients utilising the service complained of pain, a key domain of quality of life.18 Where a diagnosis was made, over three quarters of adults and nearly all child patients had pain attributable to pulpitis or a dental abscess. Just over half of all these adult and child patients received either definitive treatment or advice; the rest received antibiotics alone. Pulpitis is an inflammatory condition and local measures alone should remove the pain experienced by these patients.19 The use of antibiotics for the management of pulpitis is inappropriate as shown by several scientific studies.20,21 It was disturbing in this study that 18% of patients, especially children, received antibiotics for this reason where more localised measures should have been provided.
Where definitive management of pulpitis was provided, this was often in the form of dressings such as Ledermix™, Kalzinol™, Cavit™ and glass ionomer cements. This is well documented as the treatment of choice following the removal of decay where an acute reversible pulpitis is present, as they provide therapeutic properties and protect the pulp against further insult.22
The principal management technique for localised dentoalveolar infections, eg periapical or periodontal infection and pericoronitis, is to establish drainage by the extraction or extirpation of the offending tooth, surgical incision of a purulent swelling or irrigation of the operculum in cases of pericoronitis.23 Only 30% of the patients in this study with localised infections received definitive treatment to establish drainage of the infected material. Dry sockets should be treated with local measures achieved by the irrigation of an infected socket and packing with a dressing such as Alvogyl.24 However, over 50% of the presenting patients received antibiotics alone in the management of dentoalveolar infections and dry sockets.
Forty-three patients presenting at the clinic with pain had medical conditions which may have affected their management. Encouragingly, nearly half of these patients received appropriate treatment, but the rest received antibiotics alone. Those receiving antibiotics presented with heart murmurs, were taking warfarin or were undergoing chemotherapy. It could be speculated that the dentists did not feel comfortable or were not familiar with current guidelines in the management of patients on warfarin, or with heart conditions or receiving chemo- or radiotherapy.
The investigation also aimed to ascertain whether treatment provided by the dental clinicians was appropriate for the patients' presenting complaint. From the results it would appear that two thirds of patients received the correct treatment, based on guidelines and accepted best practice.25 As previously discussed, of some concern were the number of patients who received antibiotics for conditions such as caries, lost restorations and broken teeth. This is inappropriate treatment.23
Similarly, pericoronitis, dry sockets and periodontal abscesses can be treated effectively by local measures alone.24 Antibiotics were prescribed for eruption cysts in two instances; antibiotics are not indicated for this purpose.
A small number of patients presenting at the clinic with swellings and diagnosed as having acute dental infections received antibiotics alone. Most dental infections, unless they are severe spreading infections, should be managed immediately with drainage, eg opening a tooth to drain, incising the abscess or extracting the tooth.23 Unfortunately it would appear that definitive management of these patients was suboptimal. It is well documented that the indications for antibiotics in the treatment of acute dentoalveolar infections are well-defined clinical signs of a spreading infection, patient malaise, an elevated temperature and lymphadenitis.4,23 It is assumed that none of the infections were severe spreading infections as these patients were not referred to an accident and emergency department for emergency treatment.
The most common antibiotic prescribed was amoxicillin, either alone or in combination with metronidazole. Although both microbiological and clinical findings support the use of these antibiotics in the treatment of dental abscesses, their use should, however, only be used as an adjunct to the correct management of patients and not as treatment alone.23,26
What was also disconcerting was that 20% of patients received antibiotics where no clinical diagnosis was even made. The findings from this study therefore raise the question of whether antibiotics are being used inappropriately to treat emergency patients and if so, why?
Firstly, there could be a poor understanding among clinicians about the pathological process involved in pulpal and periapical disease, leading to incorrect diagnoses. Similarly, there could be a lack of knowledge about the correct indications for the use of antibiotics. These factors could consequently result in the inappropriate use of antibiotics and the further emergence of antibiotic-resistant strains of bacteria.
The reasons why dentists failed to provide definitive treatment and the high number of prescriptions for antibiotics in the OOH environment require further research. A number of studies in general dental practice have suggested that a lack of time and uncertainties about correct diagnosis were the main reasons for antibiotic prescribing.27,28 The treatment modalities delivered in the OOH service by dentists and the overuse and inappropriate use of antibiotics also requires further research.
Conclusions
The majority of the patients attending the OOH clinic had pain (1,201/1,472) associated with a localised infection such as pulpitis, acute dental infections and dental abscesses. Where a diagnosis was recorded, only 67% of patients received appropriate treatment. The commonest treatment provided for both adults and children was the issuing of prescriptions for antibiotics, with over half of the patients receiving antibiotics alone with no other definitive treatment provided.
The study has highlighted that many GDPs are not familiar with current clinical and best practice guidelines on patient examination, management with respect to the correct prescribing of antibiotics for dental infections, and clinical record keeping.
References
Departmentof Health. Commissioning of out of hours services and urgent treatment. London: Department of Health, 2006. Gateway reference 6990, Factsheet 7b.
The National Health Service (General Dental Services Contracts) Regulations 2005. London: The Stationery Office, 2005. Statutory Instrument 2005 No. 3361.
Palmer N O . Clinical audit of emergency out-of-hours service in general practice in Sefton. Primary Dent Care 1996; 3: 65–67.
Thomas D W, Satterthwaite J, Absi E G, Lewis M A, Shepherd J P . Antibiotic prescription for acute dental conditions in the primary care setting. Br Dent J 1996; 181: 401–404.
Dailey Y M, Martin M V . Are antibiotics being used appropriately for emergency dental treatment? Br Dent J 2001; 191: 391–393.
Standing Medical Advisory Committee. The path of least resistance. London: Department of Health, 1998.
Department of Health Statistical Division. Dental practitioner prescribing - antimicrobials, 2005. Prescription cost analysis system. London: Department of Health, 2005.
Topping G V . Out-of-hours emergency dental services - evaluation of the first year of a pilot project in Fife. Br Dent J 2005; 198: 193–197.
Portman-Lewis S. An analysis of the out-of-hours demand and treatment provided by a general dental practice rota over a five-year period. Primary Dent Care 2007; 14: 98–104.
Anderson R, Thomas D W, Phillips C J . The effectiveness of out-of-hours dental services: I. Pain relief and oral health outcome. Br Dent J 2005; 198: 91–97
Anderson R, Thomas D W, Phillips C J . The effectiveness of out-of-hours dental services: II. Patient satisfaction. Br Dent J 2005; 198: 151–156.
Anderson R . Patient expectations of emergency dental services: a qualitative interview study. Br Dent J 2004; 197: 331–334.
Burke F J, McCord J F, Cheung S W . The provision of emergency dental care by general dental practitioners in an urban area. Dent Update 1994; 21: 184–186.
Department of Health. Commissioning primary dental care services: meeting the NHS operating framework objectives. London: Department of Health, 2008. Gateway Reference 8903.
Huovinen P, Cars O . Control of antimicrobial resistance: time for action. The essentials of control are already well known. BMJ 1998; 317: 613–614.
Anon. Monitoring and management of bacterial resistance to antimicrobial agents: a World Health Organization symposium. Geneva, Switzerland, 29 November-2 December, 1995. Clin Infect Dis 1997; 24 (Suppl 1): S1–S176.
Faculty of General Dental Practice (UK). Clinical examination and record keeping: good practice guidelines. London: FGDP(UK), 2001.
Anderson R, Thomas D W . 'Toothache stories': a qualitative investigation of why and how people seek emergency dental care. Community Dent Health 2003; 20: 106–111.
Matthews R, Scully C, Porter K, Griffiths M . An analysis of conditions presenting to a dental hospital emergency clinic. Health Trends 1992; 24: 126–128.
Nagle D, Reader A, Beck M, Weaver J . Effect of systemic penicillin on pain in untreated irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 636–640.
Keenan J V, Farman A G, Fedorowicz Z, Newton J T . Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev 2005; 2: CD004969.
McDougal R A, Delano E O, Caplan D, Sigurdsson A, Trope M . Success of an alternative for interim management of irreversible pulpitis. J Am Dent Assoc 2004; 135: 1707–1712.
Faculty of General Dental Practice (UK). Adult antimicrobial prescribing in primary dental care for general dental practitioners. London: FGDP(UK), 2000.
Faculty of Dental Surgery. National clinical guidelines. London: Faculty of Dental Surgery of the Royal College of Surgeons of England, 1997.
Eaton K (ed). Standards in dentistry. London: FGDP(UK), 2006.
Canadian Collaboration on Clinical Practice Guidelines in Dentistry. Clinical practice guideline on emergency management of acute apical periodontitis in adults. Canadian Collaboration on Clinical Practice Guidelines in Dentistry, 2002. http://www.cda-adc.ca/_files/dental_profession/practising/ clinical_practice_guidelines/FULL_VERSION.pdf
Palmer N A, Pealing R, Ireland R S, Martin M V . A study of therapeutic antibiotic prescribing in National Health Service general dental practice in England. Br Dent J 2000; 188: 554–558.
Palmer N A, Dailey Y M, Martin M V . Can audit improve antibiotic prescribing in general dental practice? Br Dent J 2001; 191: 253–255.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Tulip, D., Palmer, N. A retrospective investigation of the clinical management of patients attending an out of hours dental clinic in Merseyside under the new NHS dental contract. Br Dent J 205, 659–664 (2008). https://doi.org/10.1038/sj.bdj.2008.1044
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.1044
This article is cited by
-
Behavioural intervention to promote the uptake of planned care in urgent dental care attenders: study protocol for the RETURN randomised controlled trial
Trials (2022)
-
Changes in the characteristics of dental emergencies under the influence of SARS-CoV-2 pandemic: a retrospective study
BMC Oral Health (2021)
-
Antibiotic use and resistance: a nationwide questionnaire survey among French dentists
European Journal of Clinical Microbiology & Infectious Diseases (2020)
-
Dental care provision to UK military personnel serving on Operation Herrick in Afghanistan. Part 2: aetiology and management
British Dental Journal (2019)
-
Efficacy of orally administered prednisolone versus partial endodontic treatment on pain reduction in emergency care of acute irreversible pulpitis of mandibular molars: study protocol for a randomized controlled trial
Trials (2017)